
Male inheritance
Males inherit a Y chromosome from their fathers and an X chromosome from their mothers. If they inherit an X chromosome carrying the hemophilia A gene from their mother, they will have hemophilia A.
Get more information and resources at Sanofi Rare Blood Disorders
Everyone’s hemophilia A needs are unique. More information at your fingertips can help transform how you think about and navigate what’s right for you or your child. Read on to learn about hemophilia A inheritance, common symptoms, and hemophilia A treatment options.
Hemophilia A is a rare, lifelong bleeding disorder. It’s usually inherited (passed down from parent to child) but can develop later in life, too.
People with hemophilia A have a missing or deficient clotting protein called factor VIII. Without enough of this protein, blood doesn’t coagulate like it should, which can lead to spontaneous bleeding or heavy, prolonged bleeding after an injury or surgery.
The good news: modern treatments can help manage symptoms and open up new possibilities for life with hemophilia A.
80%
of people with hemophilia have hemophilia A.


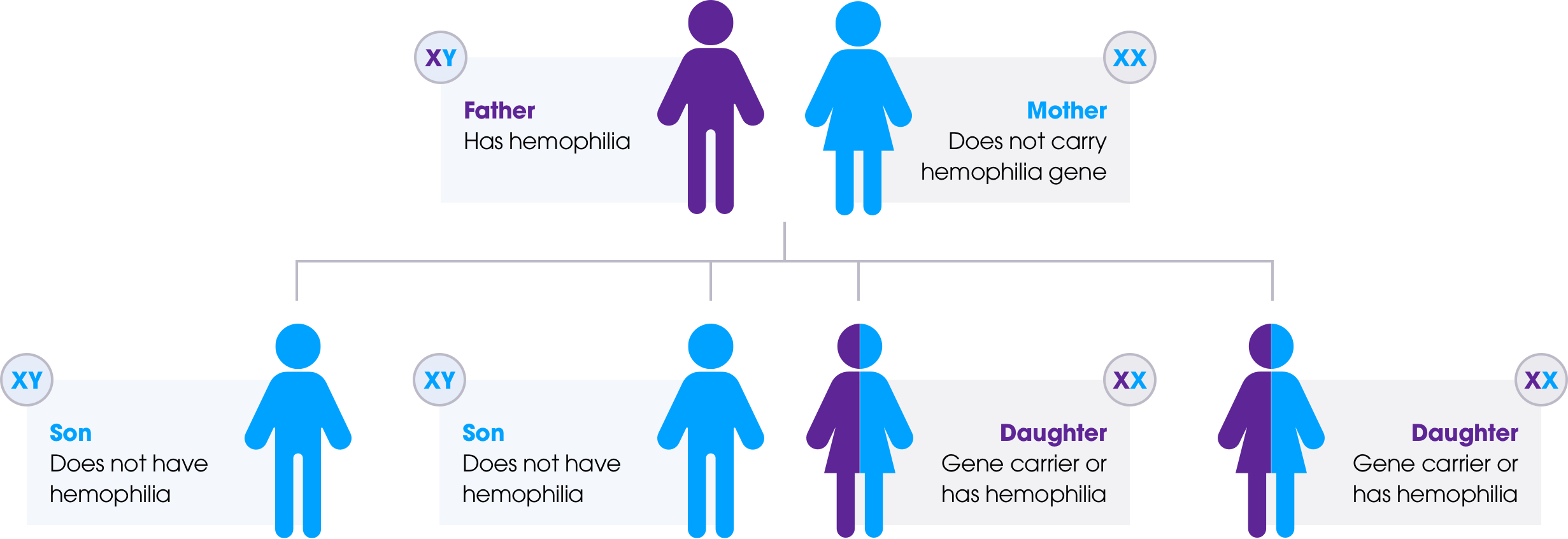
Please note: This chart is meant to help clarify the inheritance pattern of hemophilia A by aligning gender identity to both sex assigned at birth and chromosomal makeup. If your gender does not match your sex assigned at birth or if your chromosomal makeup is not represented here, talk with your care team about your inheritance risk.

Males inherit a Y chromosome from their fathers and an X chromosome from their mothers. If they inherit an X chromosome carrying the hemophilia A gene from their mother, they will have hemophilia A.

Females inherit two X chromosomes, one from their mothers and one from their fathers. If one or both of the X chromosomes carry the hemophilia A gene, they will either have hemophilia A or be a carrier. Learn more about hemophilia in women.
Common hemophilia A signs and symptoms include:
Swelling, pain, or tightness in the joints, particularly the knees, elbows, or ankles
Bleeding after having shots, which could lead to muscle bleeds
Heavy menstrual periods
Bruising on the skin
Blood in the urine or stool
Low iron levels or anemia
Bleeding in the mouth and gums that’s difficult to stop
Frequent and hard-to-stop nosebleeds
These signs and symptoms of hemophilia A can vary based on the levels of clotting factor in your blood and the hemophilia severity. If you or someone you care for is experiencing one or more of these symptoms, contact your doctor. Bleeds that go unaddressed can potentially affect joint health. Learn more about joint health and bleed management.


Phil is a promotional speaker compensated by Sanofi.
“We’ve come a long way, and I am ecstatic that there is more awareness and understanding of hemophilia than there was when I was a kid. I encourage those of you living with hemophilia to continue educating yourselves and working with your doctor to manage your hemophilia.”
Knowing what happens inside your body during a bleed can help you understand the impacts of hemophilia A—and how different treatments can help.
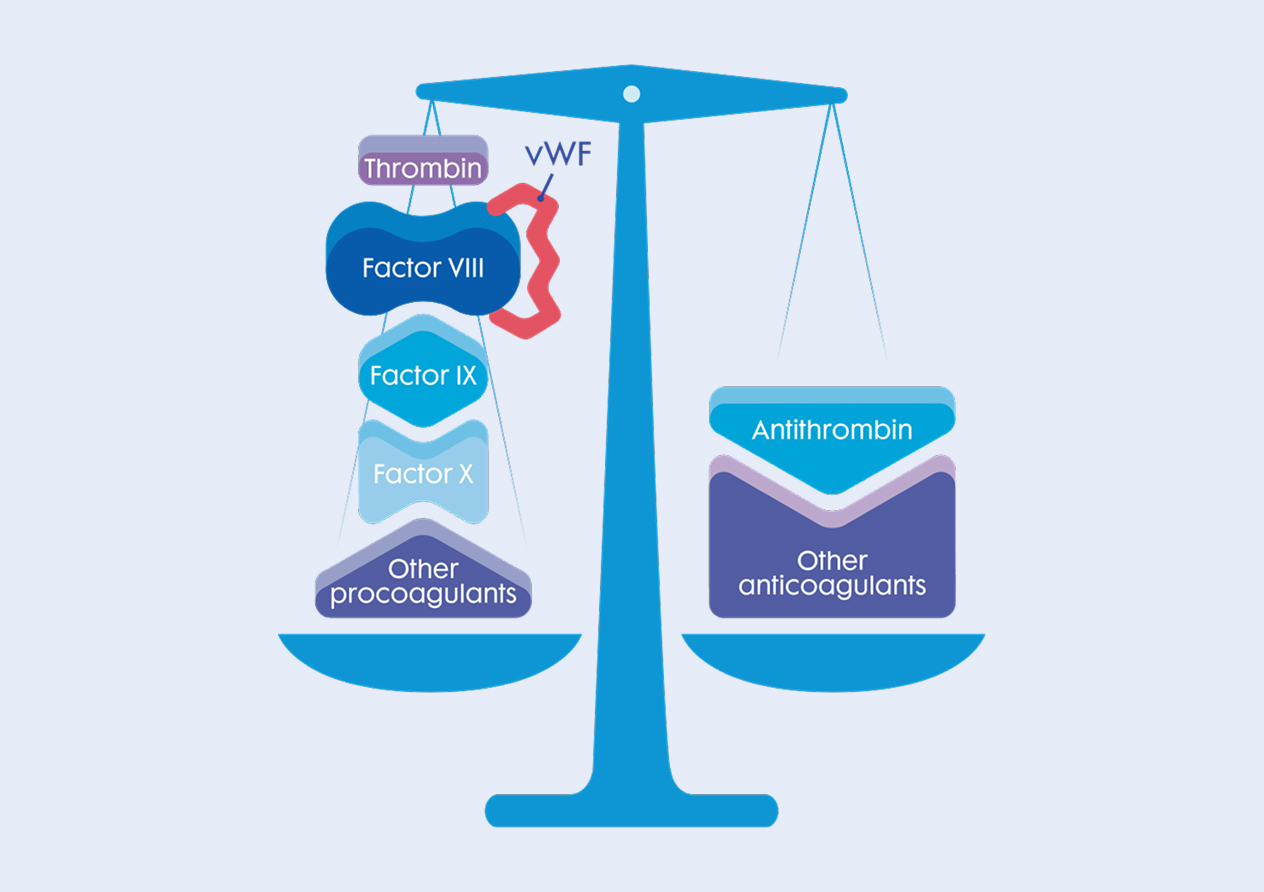
The goal: balance
Your blood contains procoagulants, which help with blood clotting, and anticoagulants, which reduce clotting to help keep blood moving through your body.
When a bleed occurs, more procoagulants are needed to help stop the bleeding and regain the balance in your body. Achieving this balance is called hemostasis, and it happens in two parts.
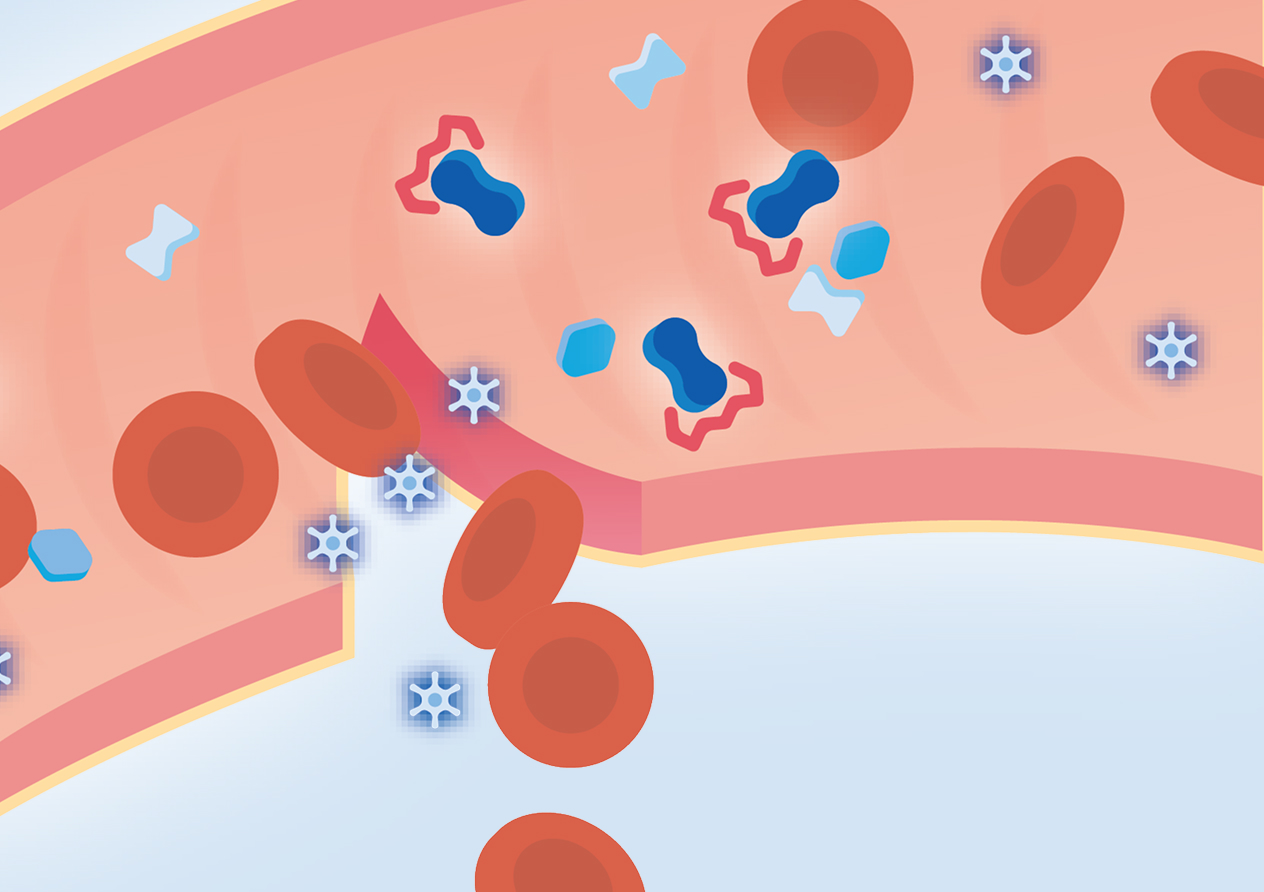
When a bleed first happens, platelets assemble at the site of the injury and create an initial clot called a “platelet plug” to slow the bleeding.
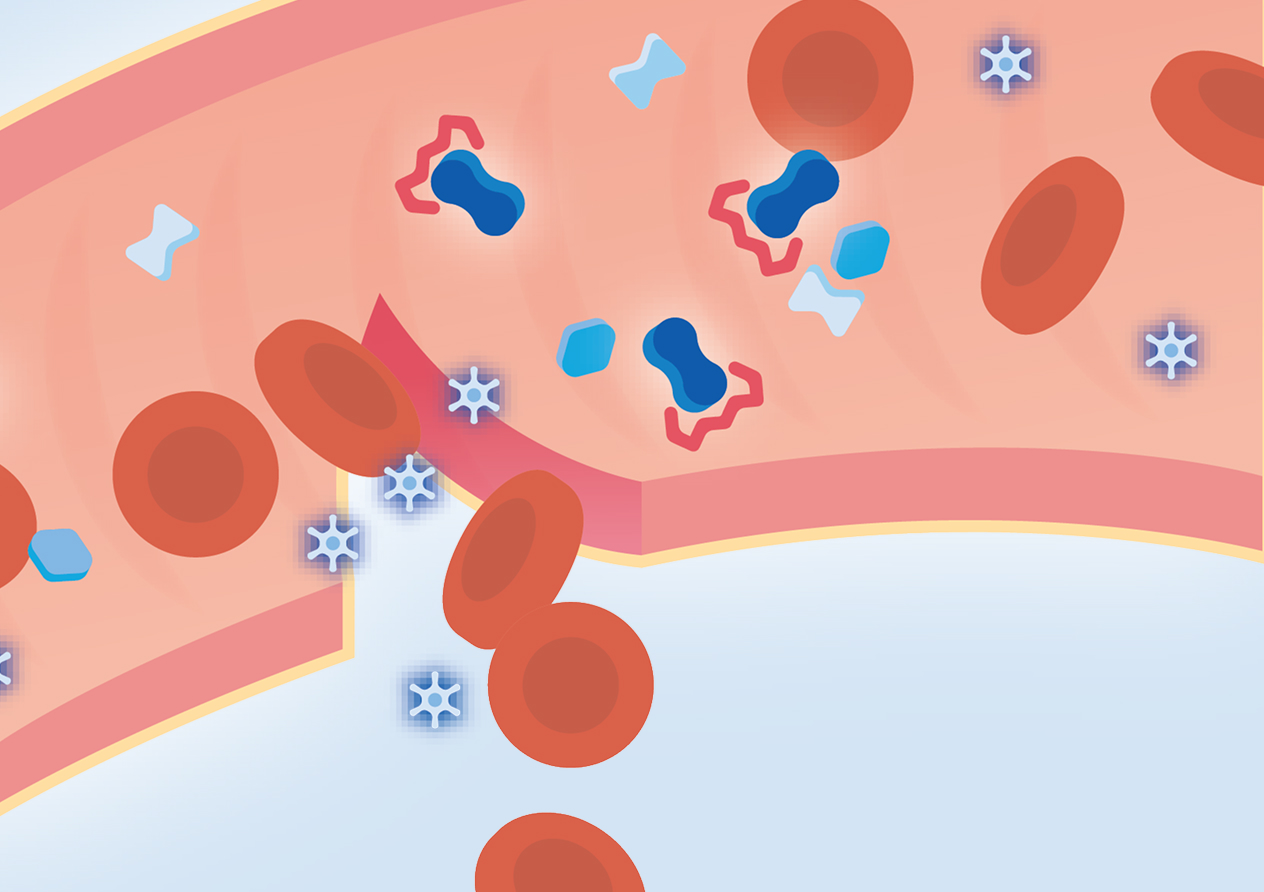
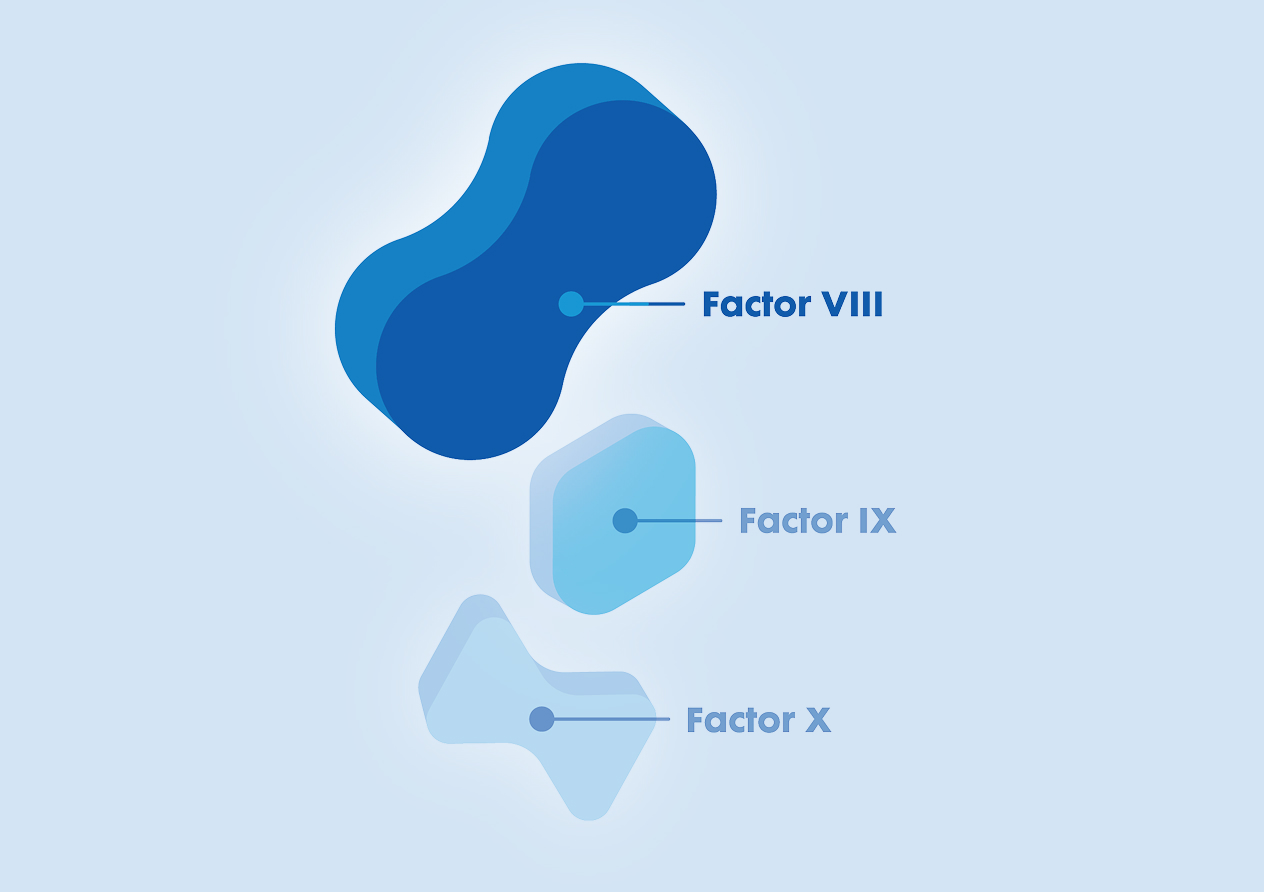
After the platelet plug forms, a multistep process called the clotting cascade is activated to help bind the platelets together and stabilize the clot.
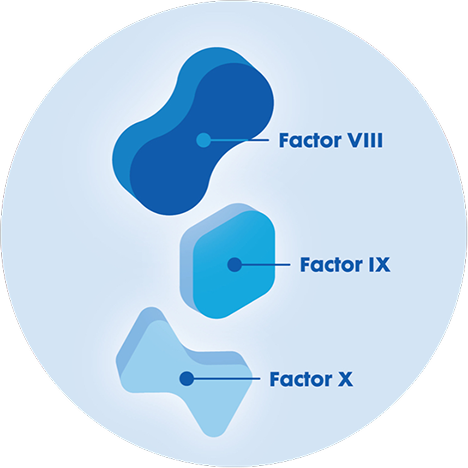
Several clotting proteins become activated, including factor VIII.
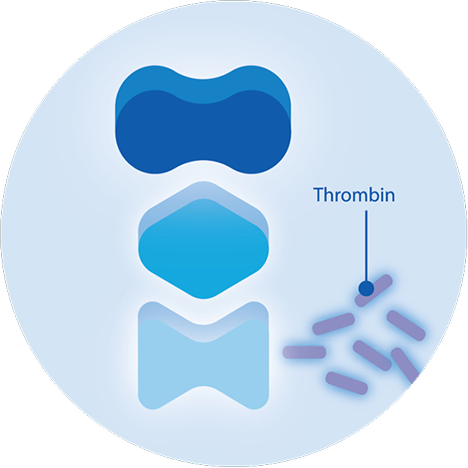
After all of the clotting proteins are activated, they work together to generate thrombin, which is necessary to form a stable clot.
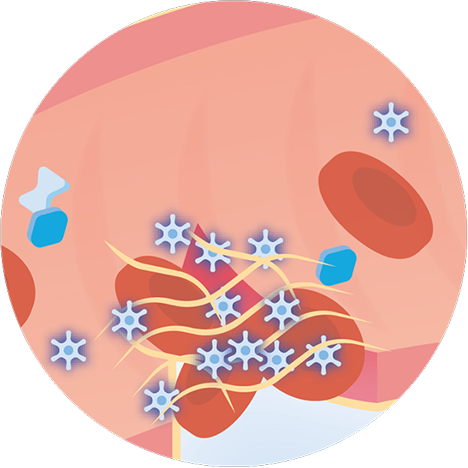
Once thrombin is activated, it helps create the crucial fibrin mesh that spreads over the platelets, binding them together into the stable clot that stops the bleeding.
Factor VIII is one of several proteins needed to form stable blood clots. But when there isn’t enough factor VIII in the blood, the clotting cascade doesn’t produce enough thrombin to achieve hemostasis and a stable clot. This can lead to excessive or uncontrolled bleeding.
Primary hemostasis
When a bleed first happens, platelets assemble at the site of the injury and create an initial clot called a “platelet plug” to slow the bleeding.

Hemophilia A treatments are all designed to help the body achieve hemostasis, but in different ways. The right hemophilia treatment depends on your factor activity levels, whether or not you have hemophilia inhibitors, and your lifestyle and treatment goals.
Learn more about Sanofi treatments for hemophilia A:
Discover an extended half-life factor replacement therapy.
LEARN MORE
Explore a non-factor therapy for people with or without inhibitors.
LEARN MORE