
Male inheritance
Males inherit a Y chromosome from their fathers and an X chromosome from their mothers. If they inherit an X chromosome carrying the hemophilia B gene from their mother, they will have hemophilia B.
Get more information and resources at Sanofi Rare Blood Disorders
Understanding what makes hemophilia B unique can help you work with your care team to develop a treatment and management plan that’s right for you or your child. Start here for facts about hemophilia B, including inheritance, symptoms, and hemophilia B treatments.
Hemophilia B is a rare, lifelong bleeding disorder. It’s usually inherited (passed down from parent to child), but can also be caused by a spontaneous gene mutation.
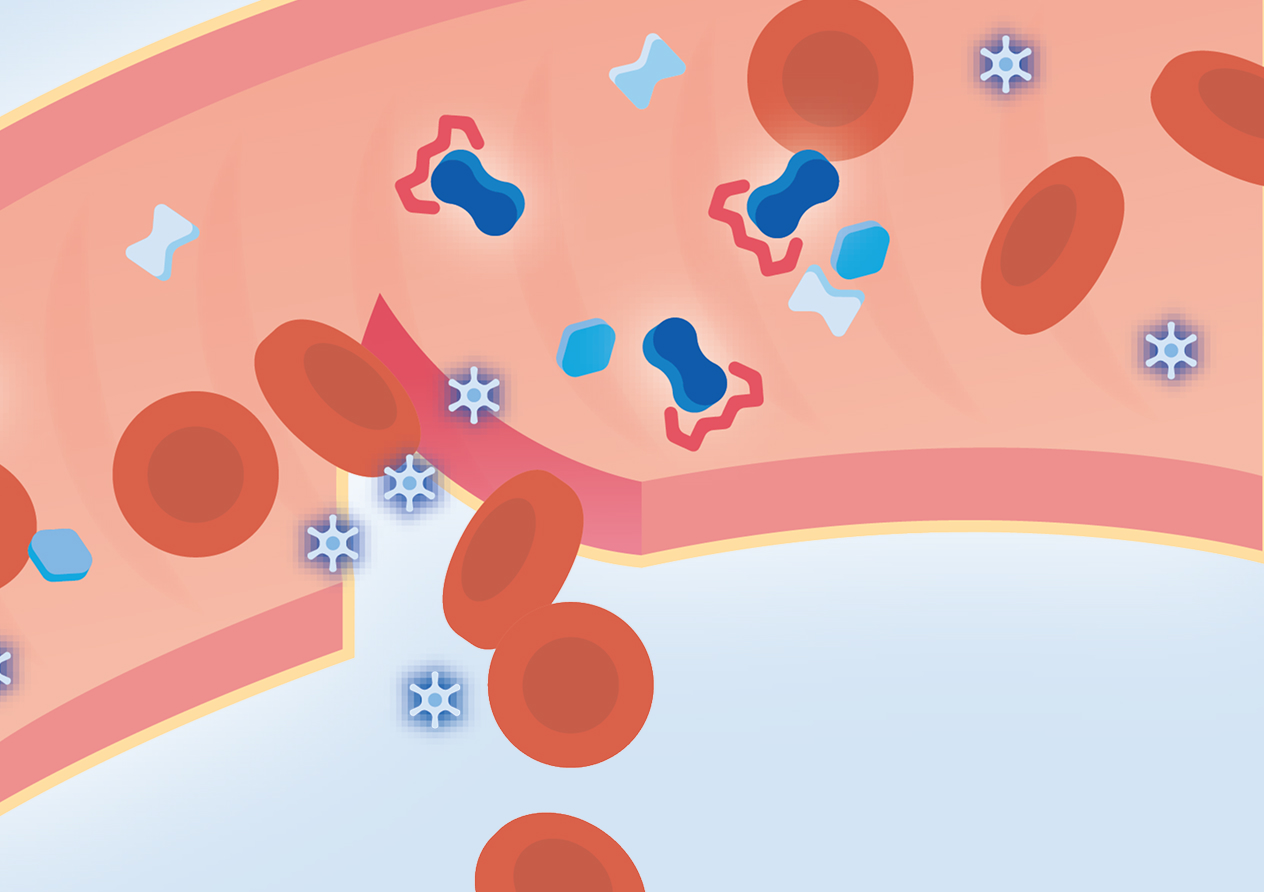
People with hemophilia B have a missing or deficient clotting protein called factor IX. Without enough of this protein, blood doesn’t coagulate like it should, which can lead to spontaneous bleeding or prolonged bleeding after an injury or surgery.
But with modern treatments, you can help manage your symptoms and shape the life you want.
1/3
of hemophilia B cases are caused by a spontaneous genetic mutation rather than being passed down from a parent.
Common symptoms of hemophilia B include:
Swelling, pain, or tightness in the joints, particularly the knees, elbows, or ankles
Bleeding after having shots, which could lead to muscle bleeds
Heavy menstrual periods
Bruising on the skin
Blood in the urine or stool
Low iron levels or anemia
Bleeding in the mouth and gums that’s difficult to stop
Frequent and hard-to-stop nosebleeds
These symptoms can vary based on the levels of clotting factor in your blood and the severity of your hemophilia. If you or someone you care for is experiencing one or more of these symptoms, contact your doctor. Bleeds that go unaddressed can potentially affect joint health. Learn more about joint health and bleed management.
“I wouldn’t be here without learning to convey my needs. Don’t be afraid to make your needs known to your healthcare team, to your family, to your friends, or to your community.”

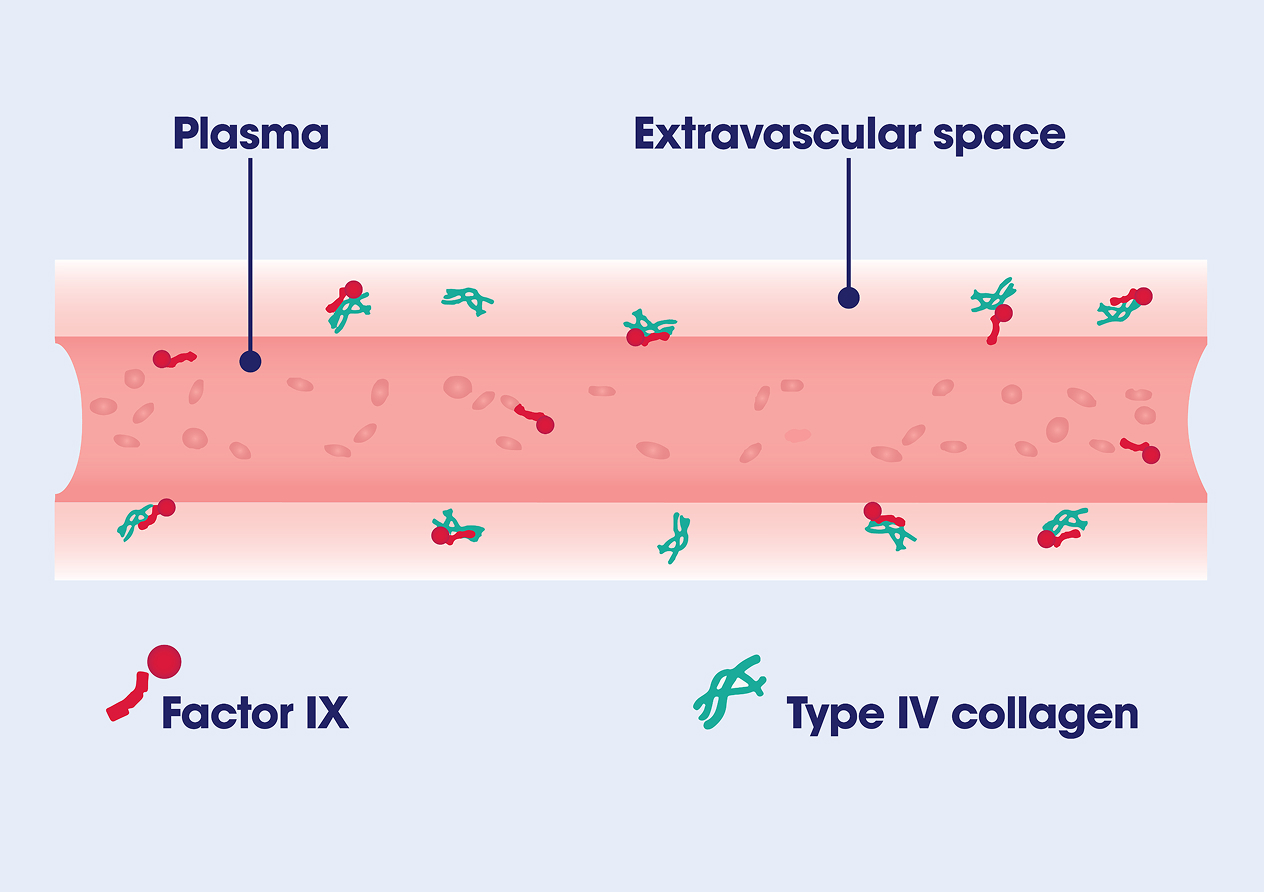
Factor IX is one of the proteins needed to form stable blood clots. Factor IX moves both in the bloodstream and outside of it, in what’s called the extravascular space. Here, it binds to type IV collagen and allows factor IX to participate in the clotting cascade to form clots and stop bleeds (learn more about the clotting cascade below).
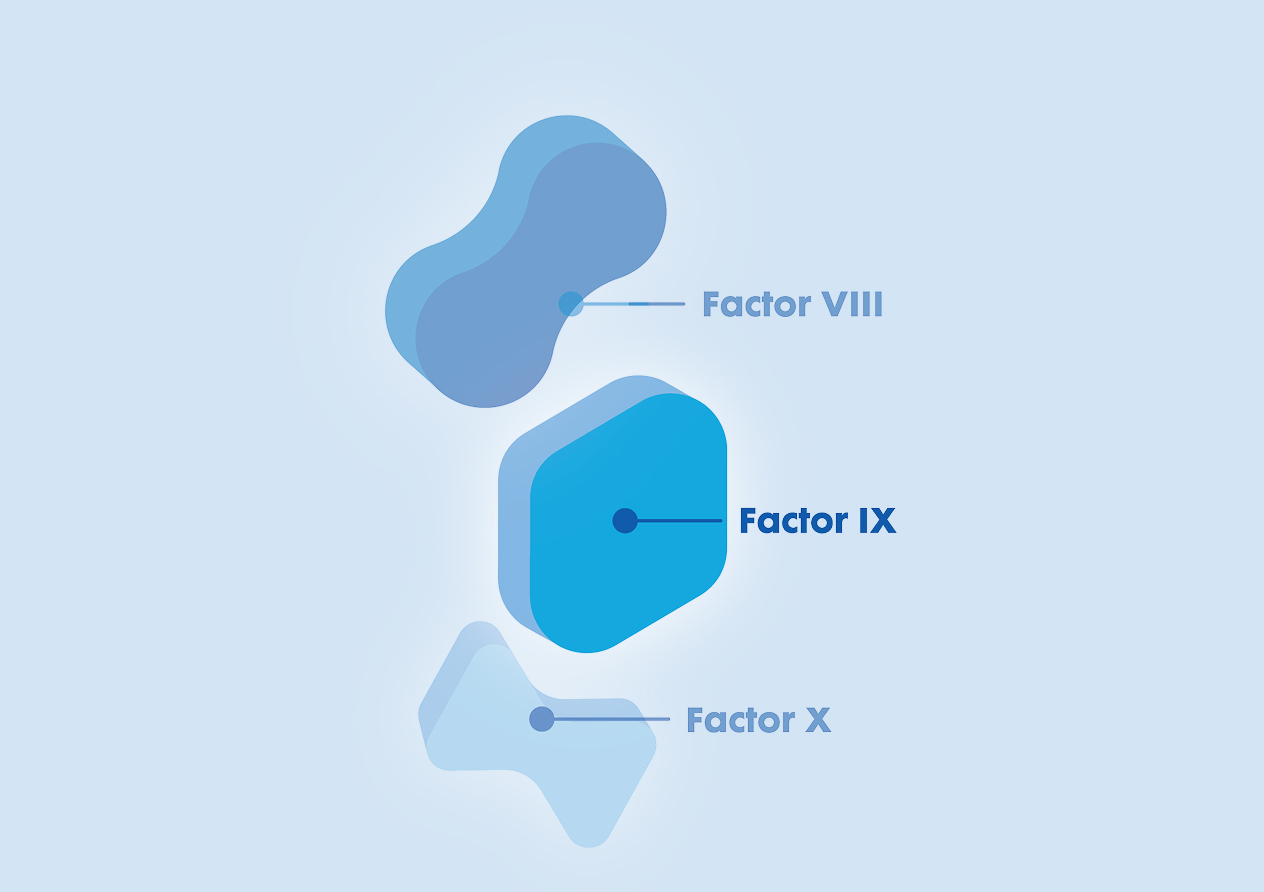
The differences between factor IX and factor VIII
Factor IX moves through the body differently than factor VIII (missing or deficient in hemophilia A), creating a unique pharmacokinetic, or PK, profile.

Half-life
This is the amount of time it takes for factor level to go down by 50% after an infusion. The half-life of factor IX tends to be longer than the half-life of factor VIII because of its extravascular distribution.

Volume of distribution
This is a measure of how much factor is in the blood and in other tissues in the body. Volume of distribution tends to be higher in factor IX than factor VIII.

Clearance
This is the speed at which factor is eliminated from the body. Factor IX clearance is higher than factor VIII clearance.

Trough
This is the lowest level of factor activity right before an infusion. For people with hemophilia B, trough may not account for all the factor IX activity in the body due to the way factor IX circulates.
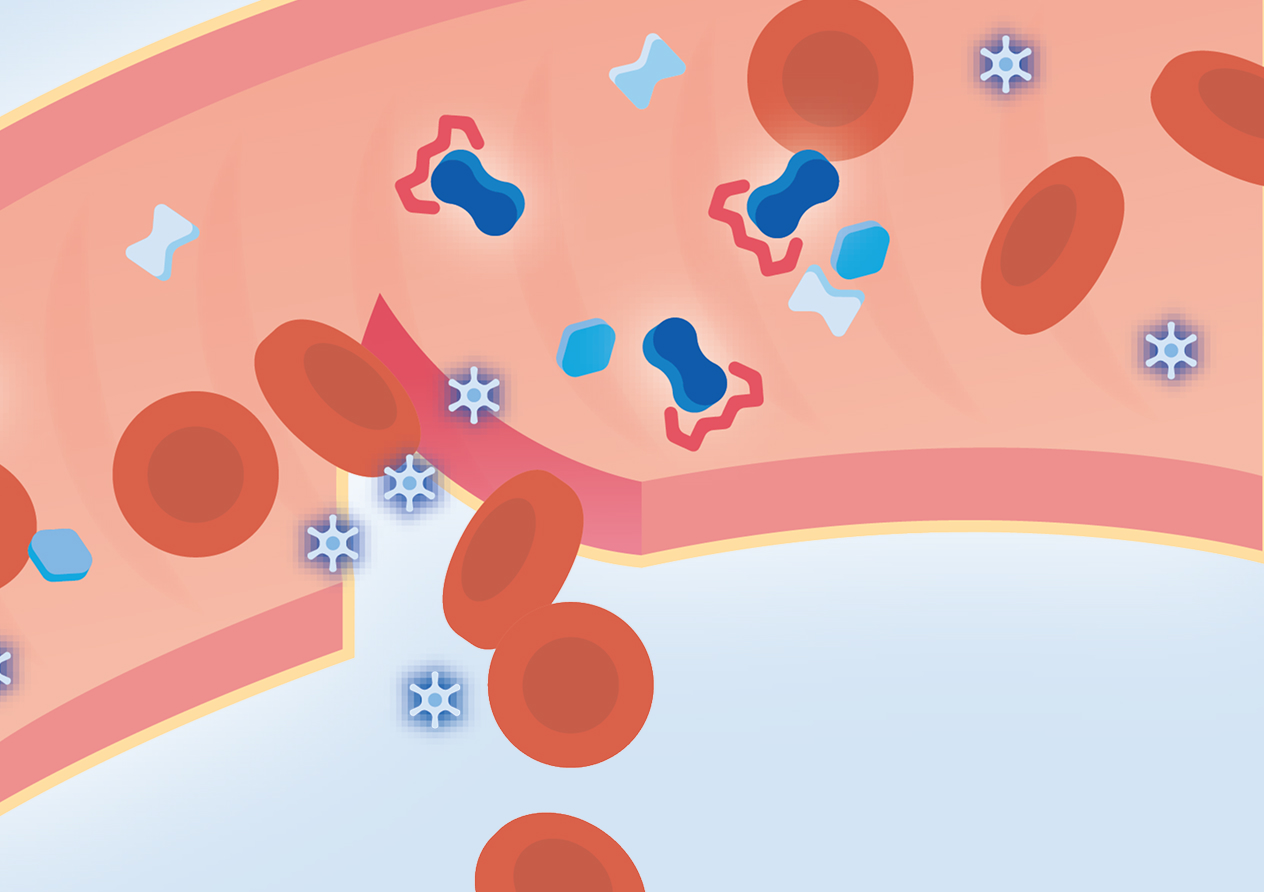
When a bleed first happens, platelets assemble at the site of the injury and create an initial clot called a “platelet plug” to slow the bleeding.
After the platelet plug forms, a multistep process called the clotting cascade is activated to help bind the platelets together and stabilize the clot.
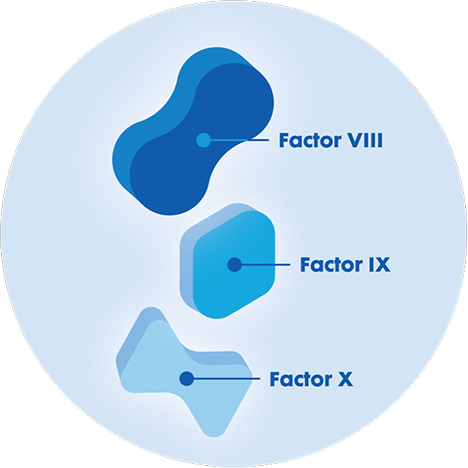
Several clotting proteins become activated, including factor VIII.
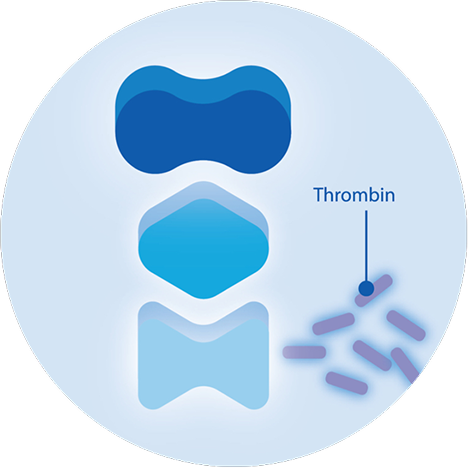
After all of the clotting proteins are activated, they work together to generate thrombin, which is necessary to form a stable clot.
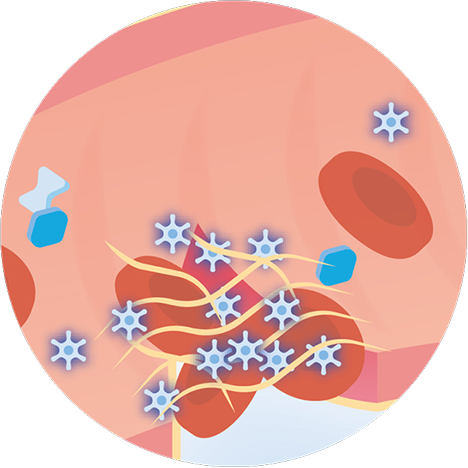
Once thrombin is activated, it helps create the crucial fibrin mesh that spreads over the platelets, binding them together into the stable clot that stops the bleeding.
If there isn’t enough factor IX in the body, the clotting cascade isn’t able to produce enough thrombin to achieve hemostasis and a stable clot. This can lead to excessive or uncontrolled bleeding.
Primary hemostasis
When a bleed first happens, platelets assemble at the site of the injury and create an initial clot called a “platelet plug” to slow the bleeding. However, this clot is unstable, and the platelets need help sticking together.

All hemophilia B treatments are designed to help achieve hemostasis quickly following a bleed, though each works in different ways. The right treatment for you depends on whether or not you have inhibitors as well as your own treatment goals and lifestyle considerations.
Your unique pharmacokinetic (PK) profile matters, too. For people with hemophilia A, trough levels are often used to help inform infusion frequency. Since factor IX can exist outside of the bloodstream, trough levels may not always reveal how much factor is in your body. A more comprehensive PK assessment is often recommended for people with hemophilia B.
Learn more about Sanofi treatments for hemophilia B:
Discover an extended half-life factor replacement therapy.
LEARN MORE
Explore a non-factor therapy for people with or without inhibitors.
LEARN MORE